Traumatic Brain Injury
A Traumatic Brain Injury (TBI) occurs when the head experiences a forceful bump, blow, or jolt, or when an object pierces the skull and enters the brain. It’s important to note that not every blow or jolt to the head results in a TBI. Whether caused by a penetrating injury like a gunshot wound or a non-penetrating incident such as a head impact in a car accident, TBIs are diverse in their origins.
These injuries vary in severity, with some individuals recovering within days, while more severe cases can lead to permanent brain damage or, tragically, result in death. Understanding the intricacies of traumatic brain injuries is crucial for effective prevention, timely diagnosis, and successful rehabilitation. In this article, we will delve into the different aspects of TBI, exploring its causes, diagnosis, treatment, and the impact it has on individuals across various age groups.
Types of Traumatic Brain Injury
Traumatic Brain Injuries (TBIs) manifest in different types, each presenting unique challenges and characteristics. Understanding these distinctions is vital for accurate diagnosis and appropriate treatment. The two primary types of TBI are:
Closed Brain Injury
Closed brain injuries occur without any break in the skull. They result from nonpenetrating injuries to the brain, typically caused by rapid forward or backward movements and shaking of the brain within the bony skull. This movement leads to bruising and tearing of brain tissue and blood vessels. Closed brain injuries commonly stem from events like car accidents, falls, sports-related incidents, and tragically, shaking a baby can also result in this type of injury, known as shaken baby syndrome.
Penetrating Brain Injury
Penetrating, or open head injuries, occur when there is a break in the skull, allowing an external object to enter the brain. This can happen in instances such as gunshot wounds, where a bullet pierces through the skull, causing direct trauma to the brain. Penetrating brain injuries often result in distinct challenges due to the direct impact on brain tissue and surrounding structures.
Symptoms

Mild Traumatic Brain Injury
Physical Symptoms
Sensory Symptoms
Cognitive, Behavioral, or Mental Symptoms
Moderate to Severe Traumatic Brain Injuries
In addition to the symptoms of mild injury, moderate to severe TBIs may exhibit the following:

Physical Symptoms
Cognitive or Mental Symptoms
Children’s Symptoms
Recognizing TBI symptoms in children can be challenging, but parents and caregivers should be vigilant for:


Causes
Traumatic Brain Injuries (TBIs) can result from various causes, each contributing to changes in chemical and energy use in the brain as a compensatory mechanism for the injury. These changes, often triggered by violent and forceful impacts to the head, may lead to symptoms such as headaches, sensitivity to light and sound, and confusion. While mild TBIs may see short-lived changes without permanent brain damage, severe injuries can have prolonged effects, causing damage to brain cells and contributing to brain swelling.
These are the top causes of traumatic brain injuries (TBIs):
Diagnosis and Tests
Diagnosing a traumatic brain injury (TBI) involves a comprehensive assessment by healthcare professionals to understand the extent and nature of the injury. The diagnostic process includes the following components:
Neurological Evaluation
Conducted by a neurologist, a specialist in the brain, a neurological evaluation assesses various aspects of brain function. This includes an examination of memory, cognitive abilities, motor function (including balance, reflexes, and coordination), and sensory functions such as hearing and vision. The goal is to gauge the impact of the injury on different aspects of the patient’s neurological health.
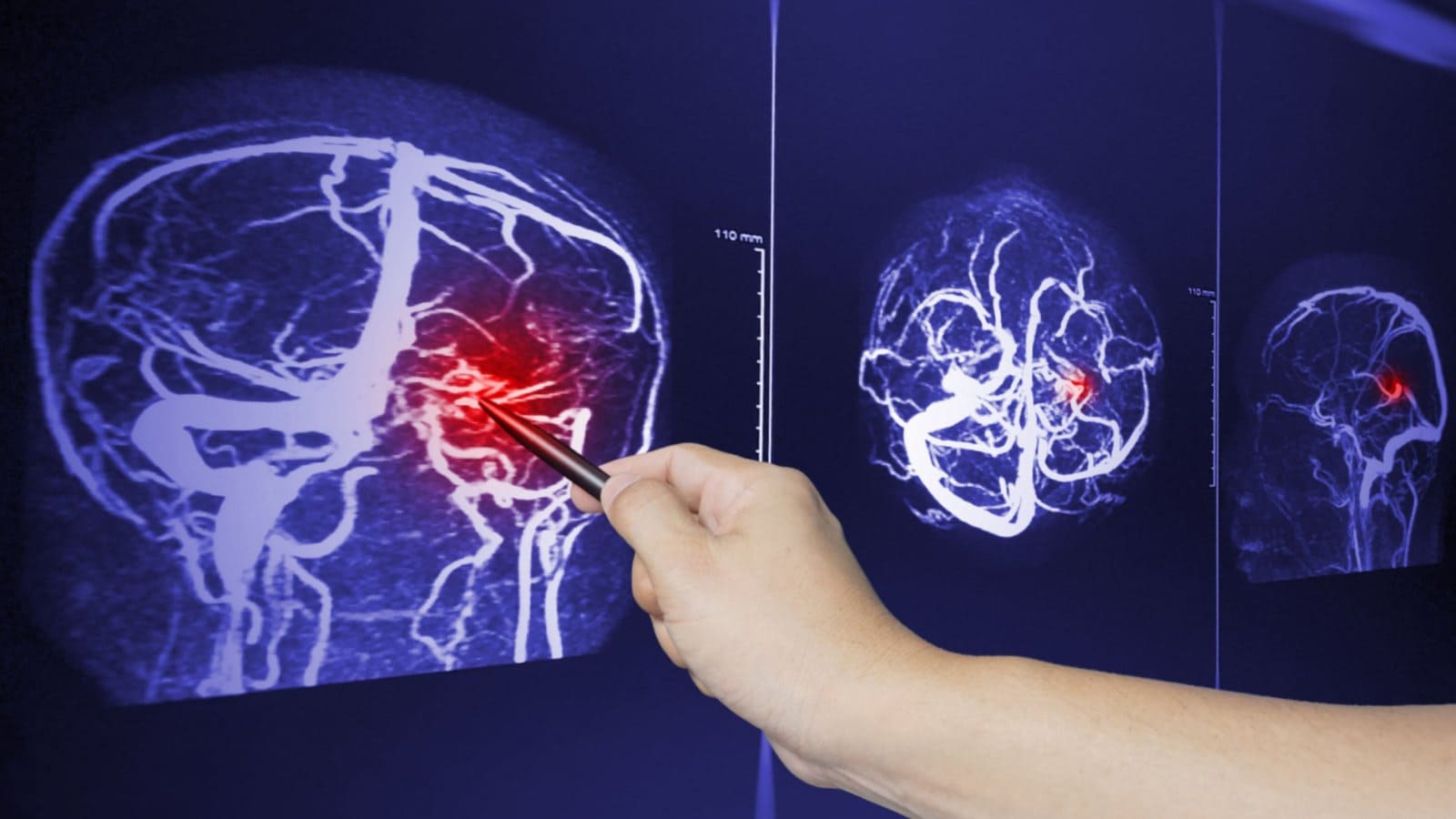
Imaging Tests
To visualize and identify potential abnormalities in the brain, imaging tests are often employed. Both CT (computed tomography) scans and MRI (magnetic resonance imaging) are utilized to check for brain bleeding and swelling. These tests provide detailed images that aid in diagnosing the severity and specific characteristics of the traumatic brain injury.
Blood Test
An innovative tool in TBI diagnosis is the Banyan Brain Trauma Indicator™ (BTI). This blood test searches for specific proteins indicative of concussion or mild TBI. The results help healthcare providers to corroborate clinical observations and imaging findings, contributing to a more comprehensive understanding of the injury’s impact on the brain.
The combination of these diagnostic approaches enables healthcare professionals to make informed decisions regarding the severity of the traumatic brain injury and formulate an appropriate treatment plan tailored to the individual needs of the patient.
Management and Treatment
The approach to managing and treating Traumatic Brain Injury (TBI) depends on various factors, including the size, severity, and location of the brain injury. These elements significantly influence the treatment strategy and the potential speed of recovery. Here’s a breakdown of the management and treatment approaches for different levels of TBI

Mild TBI
For individuals with mild TBI, such as a concussion, treatment typically involves:
Medications may include:
Severe TBI
Immediate treatment for severe TBI focuses on preventing immediate threats to life and stabilizing vital organ functions. This includes:
In-hospital strategies for managing severe TBI aim to prevent conditions including:
Additional considerations for severe TBI management:
Rehabilitation includes:

Factors influencing recovery

Prevention
Preventing Traumatic Brain Injuries (TBIs) is paramount, and various measures can significantly reduce the risk of sustaining a head injury. Unlike many neurological disorders, TBIs are largely preventable. The Centers for Disease Control and Prevention (CDC) recommends the following actions to minimize the occurrence of TBIs:
When to See a Doctor
It’s crucial to consult with a healthcare professional under specific circumstances to ensure prompt and appropriate care for potential traumatic brain injuries (TBIs). Consider the following guidelines on when to see a doctor: