Stroke
A stroke is a life-threatening event that occurs when a portion of the brain is deprived of adequate blood flow. This often results from a blocked artery or bleeding within the brain. The consequences are dire, as brain cells in the affected area begin to perish due to insufficient oxygen.
IMPORTANT NOTE: A stroke is a critical emergency where each passing second holds significant importance. If you, or someone around you, exhibits symptoms of a stroke, dial 911 (or your local emergency services number) without delay. Swift treatment substantially increases the likelihood of recovery without lasting disability.
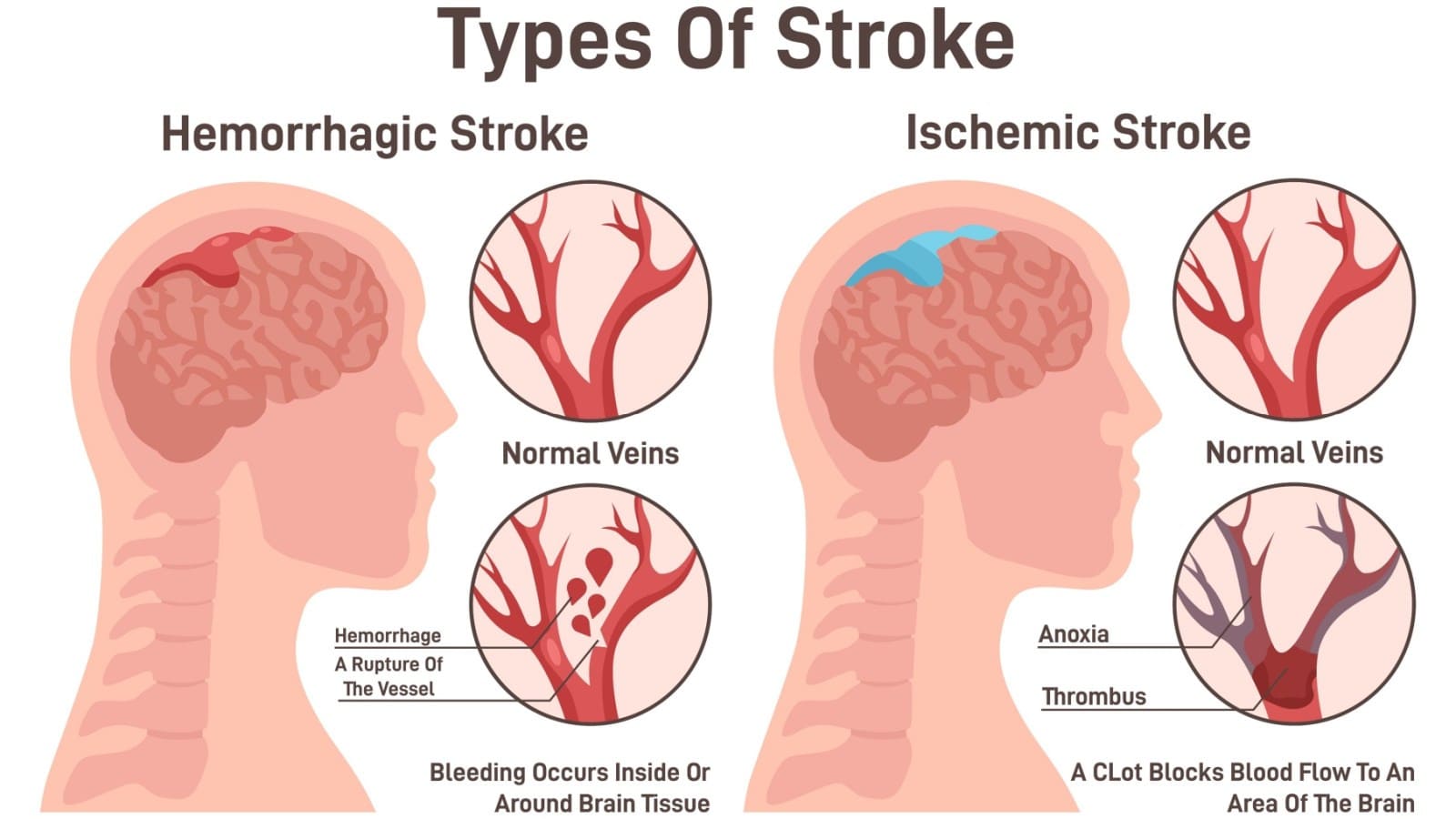
Identifying Warning Signs: The BE FAST Method
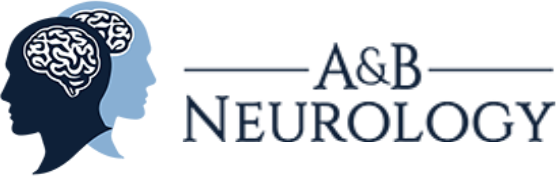
Types of Stroke
Ischemic Stroke
Hemorrhagic Stroke
Transient Ischemic Attack (TIA)
Understanding the types of strokes is crucial for accurate diagnosis and tailored treatment approaches. This knowledge empowers individuals to take proactive measures in stroke prevention and timely response.
Symptoms
When to See a Doctor
If you notice any symptoms of a stroke, no matter how fleeting they may seem, seek immediate medical attention. Call 911 or your local emergency number without hesitation. Waiting to see if symptoms resolve on their own is not an option. Every minute plays a pivotal role, and delaying treatment increases the risk of irreversible brain damage and disability.
If you are with someone showing signs of a stroke, closely monitor them while awaiting emergency assistance. Time is of the essence, and swift action is the key to a more favorable outcome in the face of this medical emergency.
Risk Factors

Lifestyle Risk Factors
Medical Risk Factors
Other Contributing Factors
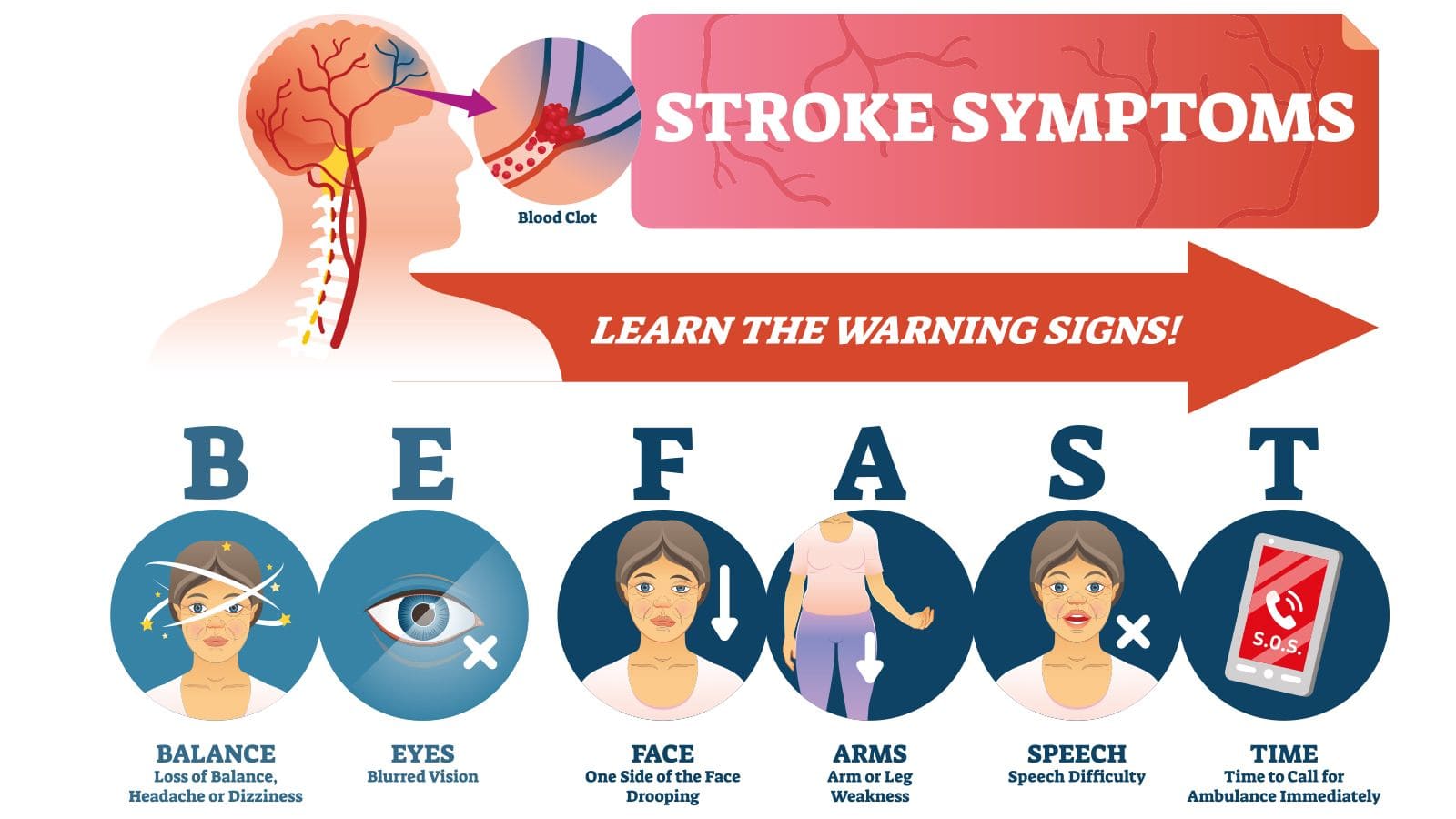
Diagnosis and Tests
Neurological Examination
Healthcare providers employ a neurological examination, observing tasks and responses to identify signs of brain dysfunction.
Key Diagnostic Tests
Understanding strokes, their symptoms, and the diagnostic process empowers individuals to take swift action. Remember, time is critical in stroke care, and immediate attention can make a significant difference in the journey to recovery.
Management and Treatment
Emergency Response
Upon recognizing stroke symptoms, the first step is to call 911 or your local emergency services number. Quick transportation to a medical facility equipped to handle strokes is essential.
Diagnostic Confirmation
Healthcare providers conduct a series of tests, including a neurological examination, CT scan, lab blood tests, electrocardiogram (ECG or EKG), magnetic resonance imaging (MRI) scans, and, if needed, an electroencephalogram (EEG). These help confirm the stroke type and severity.
Treatment Approaches
Ischemic Stroke Treatment
For ischemic strokes, where blood flow is blocked, the primary treatment is administering clot-busting medications such as tissue plasminogen activator (tPA). Mechanical thrombectomy, a procedure to remove blood clots, might also be considered in certain cases.

Hemorrhagic Stroke Management
In cases of hemorrhagic strokes, where bleeding occurs, treatment involves controlling the bleeding and reducing pressure on the brain. This may include surgery to repair blood vessel abnormalities or remove blood from the brain.
Post-Stroke Care: Building a Foundation for Recovery
Rehabilitation and Support
Physical Therapy
Rehabilitation plays a pivotal role in the post-stroke journey. Physical therapy focuses on restoring motor skills, strength, and coordination, promoting independence in daily activities.
Speech and Language Therapy
For those experiencing speech difficulties post-stroke, speech and language therapy aids in regaining communication skills and addressing swallowing issues.
Occupational Therapy
Occupational therapy helps individuals regain independence in activities of daily living, enhancing overall quality of life.
Medication Management
Controlling Risk Factors
Medications may be prescribed to manage underlying risk factors such as high blood pressure, high cholesterol, and diabetes, reducing the likelihood of future strokes.
Anticoagulants and Antiplatelets
For certain individuals, anticoagulant or antiplatelet medications may be recommended to prevent blood clots and reduce the risk of recurrent strokes.


Prevention
Many stroke prevention tactics align with strategies for preventing heart disease. Embracing a healthy lifestyle involves: