Seizures
Seizures, a medical condition characterized by a temporary and uncontrollable surge of electrical activity in the brain, have been a subject of intrigue and misconception throughout history. Seizure arises when specific brain cells undergo an overwhelming release of signals, creating an electrical overload in the affected regions of the brain.
The consequences of this electrical overload are diverse, leading to a spectrum of symptoms such as abnormal sensations, loss of consciousness, and uncontrolled muscle movements. The intricacies of seizure manifestations necessitate a comprehensive understanding to tailor effective management strategies.
Contrary to ancient beliefs across multiple cultures associating seizures with possession by evil spirits or demons, modern medicine has unveiled the reality that seizures can affect anyone. Moreover, some individuals may be more predisposed to experiencing seizures than others. This article aims to unravel the complexities of seizures, shedding light on their causes, types, diagnostic approaches, and treatment options to empower individuals in navigating this intricate neurological terrain.
Types of Seizures
Seizures can manifest in various forms, and understanding the distinct types is essential for accurate diagnosis and effective management. Here, we’ll explore the two primary categories: focal seizures and generalized seizures.
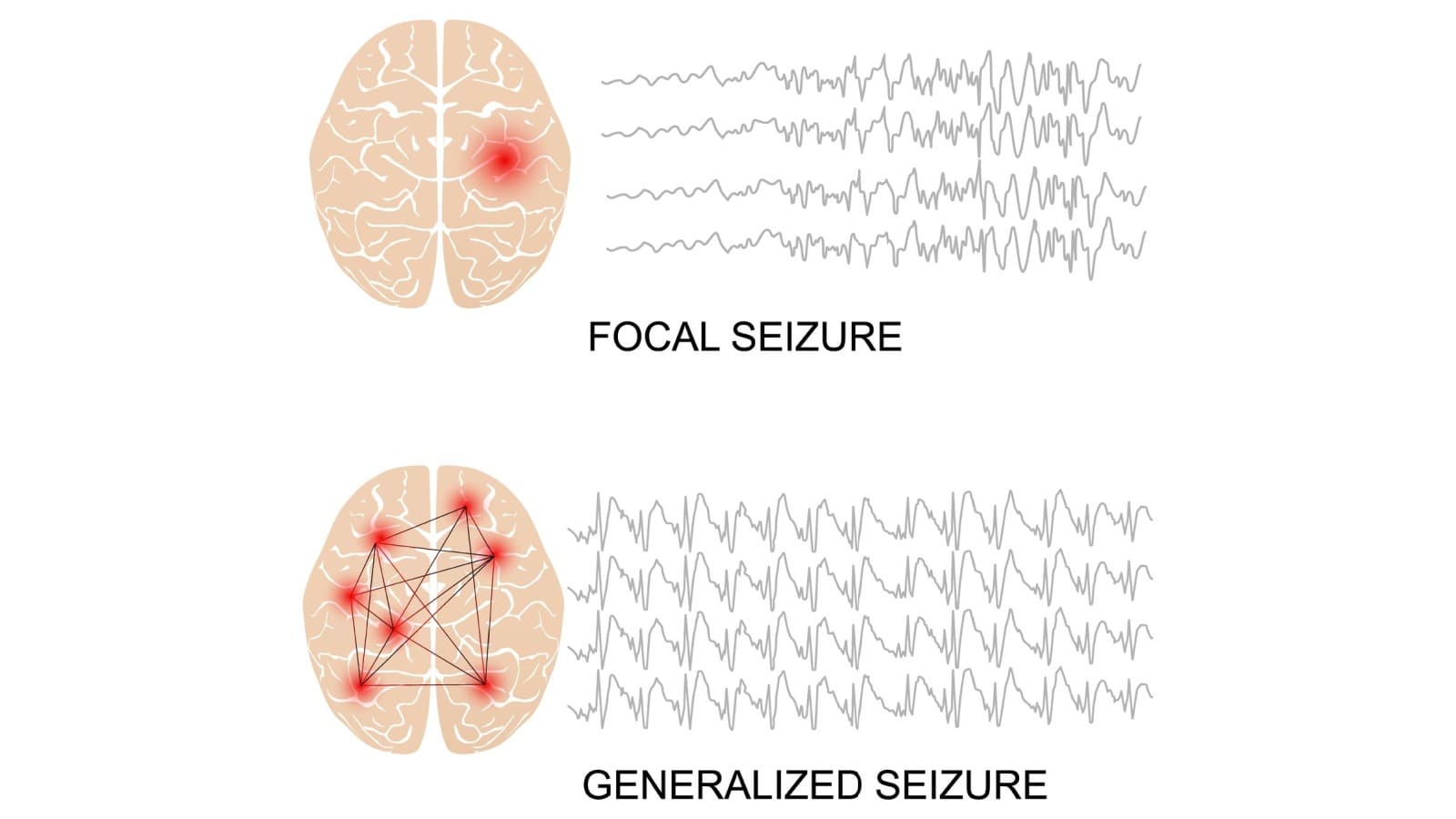
Focal Seizures
Focal seizures, also known as partial seizures, originate in a specific area of the brain. The symptoms can vary widely based on the affected region. Focal seizures are further classified into two types: simple and complex.
Generalized Seizures
Generalized seizures involve abnormal electrical activity throughout the entire brain, affecting both hemispheres. This type is characterized by widespread symptoms that often impact the entire body. There are several subtypes of generalized seizures:
Causes of Seizures
Seizures can stem from a variety of causes, encompassing:
Common Seizure Triggers for Some Individuals
Understanding these diverse triggers is crucial in developing personalized approaches to seizure management and prevention.


Signs and Symptoms
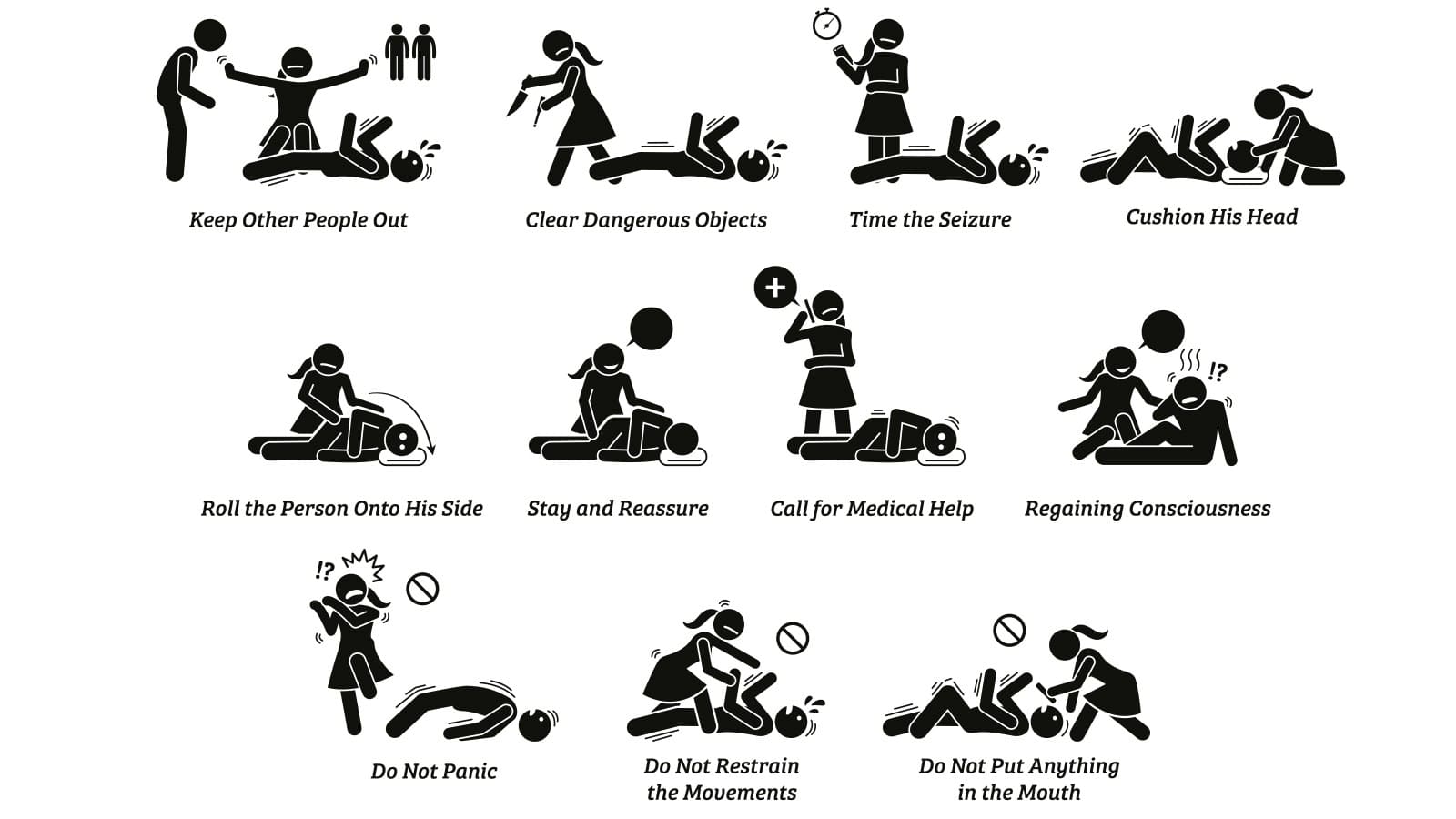
Seizure symptoms exhibit considerable variation, encompassing a sudden shift in awareness or complete loss of consciousness. Individuals may experience unusual sensations or thoughts during a seizure, adding to the complexity of the experience.
Additionally, seizures may manifest as involuntary twitching or stiffness in the body. In more intense episodes, there can be severe stiffening and limb shaking, often accompanied by a loss of consciousness—commonly referred to as convulsion.
Understanding the diverse physical symptoms is essential for both individuals undergoing seizures and those providing support.
Diagnosis and Medical Evaluation
Seeking a diagnosis for seizures involves a comprehensive process carried out by healthcare professionals, typically neurologists. The diagnostic journey possibly includes these tests:

The goal of these diagnostic tests is not only to confirm the occurrence of a seizure but also to determine its origin, especially if there’s a focal point. Identifying a specific area where seizures originate is crucial, as it significantly influences the choice of treatment strategies.
Genetic tests may also be suggested to uncover any inherited conditions contributing to seizures, providing valuable information about the nature of the seizures an individual may experience.
In the hands of skilled healthcare providers, these diagnostic tools contribute to a comprehensive understanding of the seizures, guiding the formulation of personalized and effective treatment plans tailored to the individual’s unique circumstances.
Providers may also recommend additional tests if there is suspicion of injuries, side effects, or complications arising from seizures. It is essential to trust the expertise of the healthcare provider, who will advise on the types of tests needed and the reasons behind each recommendation.
Treatment Options
Medications for Seizure Control
Medications serve as the frontline defense for individuals with epilepsy. They come in various forms, each tailored to address specific seizure types. Some medications act in real-time, halting seizures as they occur, while others work preventively, reducing the frequency of episodes. Intravenous (IV) medications offer immediate relief during a seizure, while daily oral medications provide ongoing management.
Epilepsy Surgery
In cases where medications prove ineffective, epilepsy surgery emerges as a potential solution. This procedure aims to halt seizures by removing or disconnecting the problematic brain area. Healthcare providers recommend an evaluation for epilepsy surgery if seizures persist despite trying two anti-seizure medications at recommended doses.
Dietary Changes
Dietary modifications, such as adopting low-carb or ketogenic diets, offer an alternative approach for seizure control. These specialized diets have shown the ability to either entirely stop or significantly reduce the frequency of epileptic seizures. Particularly beneficial when medications or surgery are not feasible, these diets provide a unique avenue for certain individuals.
Brain Stimulation
Two innovative forms of brain stimulation—deep brain stimulation and responsive neurostimulation—have demonstrated efficacy in seizure management. These treatments involve the implantation of a device into the brain, delivering a mild electrical current to interfere with and disrupt seizure-related electrical activity. This approach represents a cutting-edge option for those seeking alternatives to traditional treatments.
Vagal Nerve Stimulation
The vagal nerve, the 10th cranial nerve directly connected to the brain, plays a crucial role in seizure management. Electrical stimulation applied to the left side of the vagal nerve has shown promise in reducing the frequency of seizures. Vagal nerve stimulation represents a non-invasive yet impactful method, providing an additional avenue for individuals seeking diverse approaches to seizure control.
Complications and Side Effects of Treatment
The complexities and potential complications of seizure treatments are diverse, influenced by factors such as the underlying cause, seizure type, and the chosen treatment modality. Healthcare providers offer personalized insights into the likely side effects and complications based on an individual’s unique case. Seeking guidance from a healthcare professional ensures accurate and tailored information pertinent to the specific circumstances of the person undergoing treatment.