Epilepsy
Epilepsy, a neurological disorder characterized by recurrent seizures, affects millions worldwide. This article explores various facets of epilepsy, delving into types, causes, symptoms, diagnosis, and treatment, with a focus on living with the condition.
Types of Epilepsy
Focal onset seizures originate in specific brain areas, while generalized onset seizures affect the entire brain. Understanding these distinctions is crucial for accurate diagnosis and effective management.
Causes and Triggers
Understanding the causes and triggers is vital for managing epilepsy:


Symptoms of Epilepsy
Symptoms vary based on seizure types:
When to See a Doctor
If any of the following situations accompanies a seizure, it is crucial to seek immediate medical attention:

Diagnosis and Testing
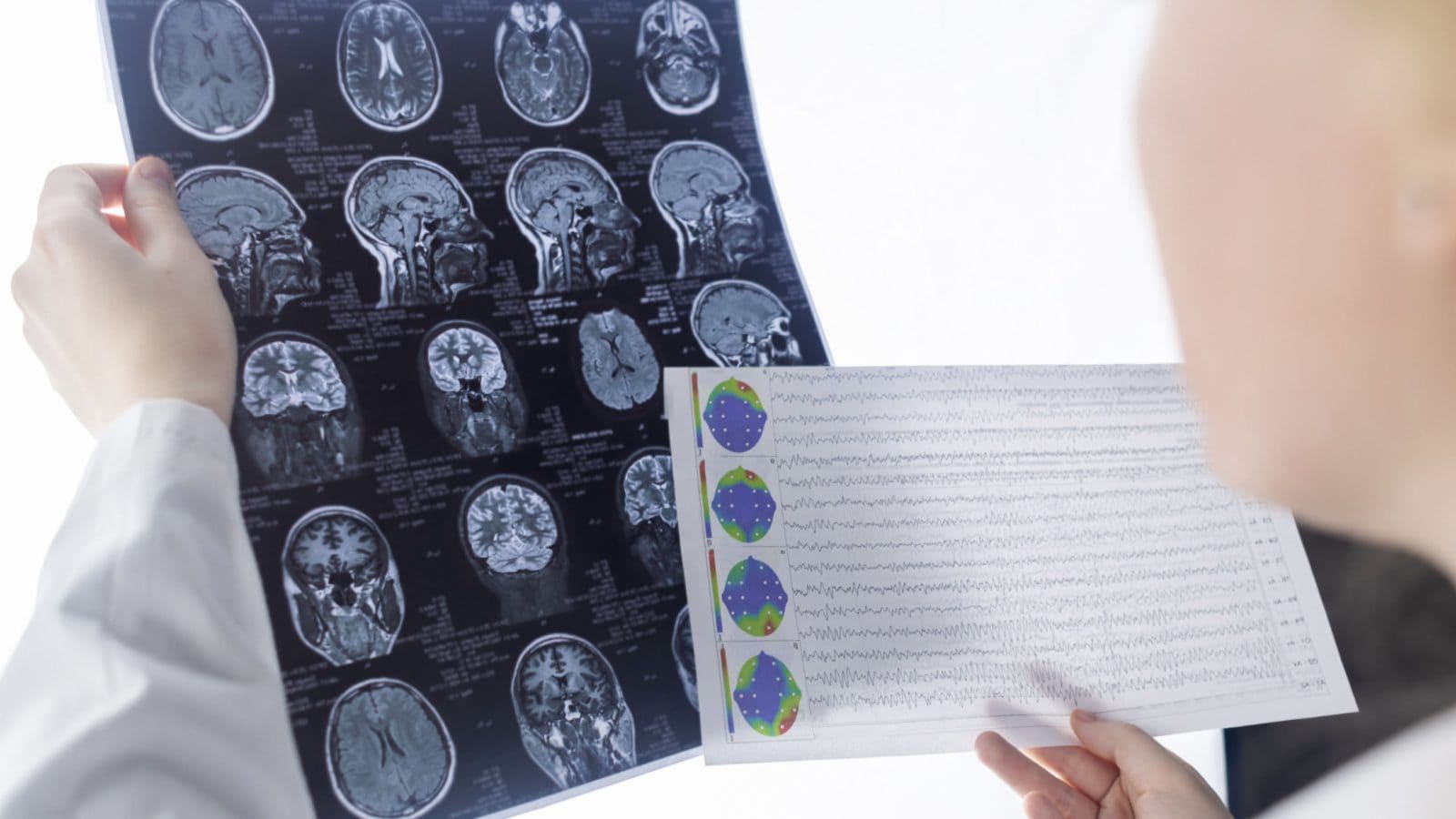
Diagnosing epilepsy involves a comprehensive approach, starting with a detailed medical evaluation. We will gather information about the individual’s medical history, symptoms, and any potential triggers. This initial assessment plays a crucial role in understanding the nature of the seizures and determining the most effective course of action.
One of the primary diagnostic tools is the electroencephalogram (EEG). This non-invasive test records the brain’s electrical activity through electrodes attached to the scalp. Abnormal patterns in the EEG can help confirm the presence of epilepsy and identify specific types of seizures.
In addition to the EEG, imaging studies such as magnetic resonance imaging (MRI) may be employed to visualize the brain’s structure. These images assist in identifying any abnormalities or lesions that could be contributing to the seizures.
The combination of medical history, EEG results, and imaging studies allows us to make a precise diagnosis and tailor an individualized treatment plan. It is important for individuals experiencing symptoms or seizures to undergo these diagnostic procedures promptly to initiate timely and appropriate interventions.
Treatment Options
Medication (Antiepileptic Drugs – AEDs):
Prescription medications, known as antiepileptic drugs (AEDs), form a cornerstone in the treatment of epilepsy. These medications are specifically designed to prevent or reduce the frequency of seizures. The choice of medication is tailored to the type of epilepsy and individual response. It involves a careful balance, with regular monitoring and adjustments made to optimize effectiveness while minimizing potential side effects.

Surgical Intervention:
In cases where medication alone proves insufficient, surgical intervention becomes a consideration. This option involves procedures such as removing or altering specific brain areas responsible for seizures. However, surgical interventions are typically reserved for situations where the potential benefits clearly outweigh associated risks.
Lifestyle Modifications:
Beyond medical interventions, lifestyle modifications play a pivotal role in managing epilepsy. This includes maintaining a regular sleep schedule, managing stress, and avoiding potential triggers. Additionally, adopting a well-balanced diet and incorporating regular exercise not only contribute to overall health but may also have a positive impact on seizure management.
Collaborative Approach:
Successful epilepsy management requires a collaborative approach between individuals and their healthcare professionals. Close collaboration ensures regular follow-up appointments for ongoing monitoring of treatment efficacy. It also fosters open communication, allowing for necessary adjustments to optimize the effectiveness of the chosen treatment plan.

Living with Epilepsy
Coping strategies and robust support systems are essential for those living with epilepsy. Lifestyle adjustments and emotional well-being are key components of managing the condition.
Coping Strategies:
Developing effective coping strategies is crucial. This includes recognizing and addressing stressors, practicing relaxation techniques, and seeking emotional support. Engaging in activities that bring joy and relaxation can contribute to overall well-being.
Medication Adherence:
Consistent adherence to prescribed medications is fundamental. Establishing a routine and using reminder tools help ensure timely medication intake, enhancing seizure control and overall treatment efficacy.
Routine Healthcare Check-ups:
Regular check-ups with healthcare professionals are essential. These appointments allow for ongoing assessment of seizure management, adjustment of treatment plans if needed, and addressing any emerging concerns.
Support Systems:
Building a strong support system is beneficial. Friends, family, and support groups provide understanding, encouragement, and practical assistance. Open communication about epilepsy helps create an environment of acceptance.
Lifestyle Adjustments:
Making certain lifestyle adjustments contributes to better seizure management. This includes maintaining consistent sleep patterns, managing stress, and avoiding potential triggers. A balanced diet and regular exercise also play integral roles in overall health.
Education and Advocacy:
Empowering oneself through education about epilepsy is empowering. Advocacy efforts, both personal and within the community, contribute to reducing stigma, increasing awareness, and fostering a supportive environment for individuals with epilepsy.
Mental Health Support:
Recognizing and addressing the impact of epilepsy on mental health is crucial. Seeking professional mental health support when needed, and practicing self-care, contributes to emotional well-being and resilience.
Workplace Considerations:
Navigating the workplace with epilepsy may involve communication with employers about potential accommodations. Understanding and asserting employee rights contribute to a supportive work environment.
Myths and Facts about Epilepsy
Dispelling common misconceptions about epilepsy is crucial for fostering understanding and empathy. Here, we delve into additional myths and facts to provide a more comprehensive view:
Myth: Epilepsy is always a visible condition.
Fact: While some seizures are noticeable, others may be subtle, involving brief lapses in consciousness or staring spells. Not all seizures result in convulsions.

Myth: People with epilepsy cannot lead normal lives.
Fact: With proper management, many individuals with epilepsy lead fulfilling lives. Education, employment, and relationships are all achievable with the right support and understanding.
Myth: Epilepsy is a rare condition.
Fact: Epilepsy is more common than perceived. It affects people of all ages, races, and backgrounds, with millions worldwide living with the condition.
Myth: Epilepsy is always a lifelong condition.
Fact: While some individuals have epilepsy throughout their lives, others may outgrow it, especially in childhood. Treatment advancements and individual cases vary.
Myth: Epilepsy is always caused by a brain injury.
Fact: While brain injuries can contribute to epilepsy, it can also result from genetic factors, infections, or developmental issues. Understanding the diverse causes helps tailor treatment plans.
Myth: Seizures are always dangerous.
Fact: While some seizures pose risks, many are manageable with appropriate treatment. First aid and a supportive environment during a seizure can significantly reduce associated risks.
Myth: Epilepsy is contagious.
Fact: Epilepsy is not contagious. It does not spread through contact or proximity. Understanding this fact is vital to reducing stigma and fostering inclusivity.
Myth: Individuals with epilepsy have intellectual disabilities.
Fact: Epilepsy and intelligence are unrelated. Many individuals with epilepsy have average or above-average intelligence. The condition does not define cognitive abilities.
Myth: Epilepsy is always a result of emotional problems.
Fact: While emotional stress can trigger seizures in some cases, epilepsy is primarily a neurological disorder with diverse causes. Emotional well-being is essential but is not the sole factor.